Cystic Fibrosis
What is Cystic Fibrosis?
Cystic fibrosis (CF) is a lifelong, inherited condition that primarily affects the lungs and digestive system. It causes the body to produce thick, sticky mucus, which can clog the airways and digestive tract. This leads to problems with breathing, digestion, and nutrient absorption.
Cystic fibrosis can also impact other parts of the body, including the pancreas, liver, reproductive system, and sweat glands. It is one of the most common life-limiting genetic conditions in the UK and affects around 1 in every 2,500 babies born.
What Causes Cystic Fibrosis?
Cystic fibrosis is caused by a fault (mutation) in the CFTR gene. A child must inherit two faulty CFTR genes, one from each parent, to develop the condition. Parents who each carry one copy of the faulty gene are known as carriers. Carriers do not have symptoms of CF themselves.
There are over 2,000 known mutations in the CFTR gene, but the most common in the UK is called F508del.
Symptoms of Cystic Fibrosis in Children
Symptoms may begin soon after birth or emerge later in infancy or early childhood. These may include:
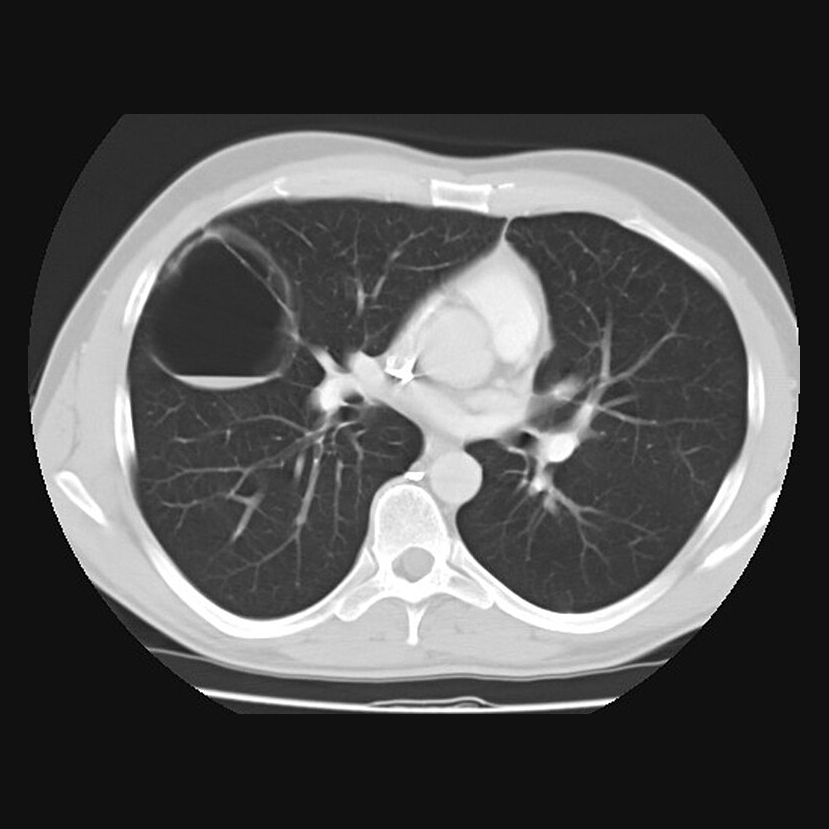
- Persistent cough with thick mucus
- Repeated chest infections or pneumonia
- Wheezing or shortness of breath
- Salty-tasting skin
- Poor growth or difficulty gaining weight
- Frequent, greasy, bulky stools or constipation
- Difficulty absorbing nutrients (due to blocked pancreatic ducts)
- Nasal polyps or chronic sinus infections
- Fertility problems (in later life, especially in males)
How is Cystic Fibrosis Diagnosed?
In the UK, all newborns are screened for cystic fibrosis as part of the newborn blood spot test (heel prick test). If the test suggests CF, further tests are performed:
- Sweat test: Measures the amount of chloride (a component of salt) in the child’s sweat. High levels indicate CF.
- Genetic testing: Confirms CF by identifying mutations in the CFTR gene.
Treatment of Cystic Fibrosis
There is currently no cure for cystic fibrosis, but advances in treatment have significantly improved quality of life and life expectancy.
Treatment plans are tailored to each child’s needs and may include:
1. Airway clearance techniques
To help clear mucus from the lungs. These may involve chest physiotherapy, percussion, or the use of a vibrating vest.
2. Inhaled medications
- Saline or mucolytics to thin mucus
- Bronchodilators to open the airways
- Antibiotics to treat or prevent lung infections
3. Enzyme and vitamin supplements
Children with CF often need:
- Pancreatic enzyme capsules with food to aid digestion
- High-calorie, high-protein diets
- Fat-soluble vitamins (A, D, E, and K)
4. CFTR modulators
These are newer, targeted drugs that improve the function of the faulty CFTR protein. Not all children are eligible, depending on their genetic mutations.
5. Regular monitoring
Children with CF require frequent check-ups, including lung function testing, weight and growth tracking, and review of treatment plans.
Living with Cystic Fibrosis
With early diagnosis, comprehensive care, and ongoing support, many children with cystic fibrosis go on to live active, fulfilling lives. Treatments have improved dramatically in recent years, with many children now living well into adulthood and beyond.
Support from a multidisciplinary team—including paediatric respiratory consultants, physiotherapists, dietitians, and CF nurse specialists—is essential.
Located in London | Infants to young adults seen
Request a referral or book an appointment with Professor Gupta today.
