Chronic Suppurative Lung Disease (CSLD) in Children
Chronic Suppurative Lung Disease (CSLD) refers to a long-term condition in which children experience ongoing infection and inflammation in the lungs, leading to the production of pus and damage to the airways. Unlike acute infections like pneumonia, which typically resolve with antibiotics, CSLD causes persistent coughing, recurring infections, and long-term structural changes in the lungs.
One of the most common consequences of untreated or severe CSLD is bronchiectasis – a condition in which the airways (bronchi) become permanently widened, scarred, and prone to recurrent infections.
Causes of Chronic Suppurative Lung Disease
CSLD can result from a range of underlying conditions that either predispose the lungs to infection or impair the body’s ability to clear mucus and fight off germs. Common causes include:
- Recurrent respiratory infections (e.g. repeated pneumonia)
- Cystic Fibrosis
- Primary Ciliary Dyskinesia (PCD) – a rare condition affecting the function of tiny hair-like structures in the lungs
- Primary or acquired immunodeficiency – when the body has trouble fighting infections
- Post-infectious damage, including following severe or poorly treated tuberculosis (TB)
- Allergic Bronchopulmonary Aspergillosis (ABPA) – a hypersensitivity reaction to a fungus
- Recurrent aspiration – where food or liquids accidentally enter the lungs (often due to swallowing difficulties)
Symptoms of CSLD in Children
Symptoms vary by age and severity, but may include:
- Chronic productive cough, often bringing up thick yellow or green mucus
- Frequent chest infections (with fevers, increased coughing or need for antibiotics)
- Wheezing or breathlessness, particularly with exercise
- Fatigue or reduced energy levels
- Poor growth and weight gain
- Clubbing (bulbous appearance of the fingertips or toes due to chronic low oxygen)
How Is CSLD Diagnosed?
If a child has had frequent chest infections, a persistent wet cough, or signs of poor lung function, your paediatrician may investigate for CSLD.
Diagnostic steps typically include:
- Detailed history and examination – looking for clues about underlying causes (e.g. family history, previous infections, immune problems)
- Chest X-ray – may show signs of persistent infection or airway changes
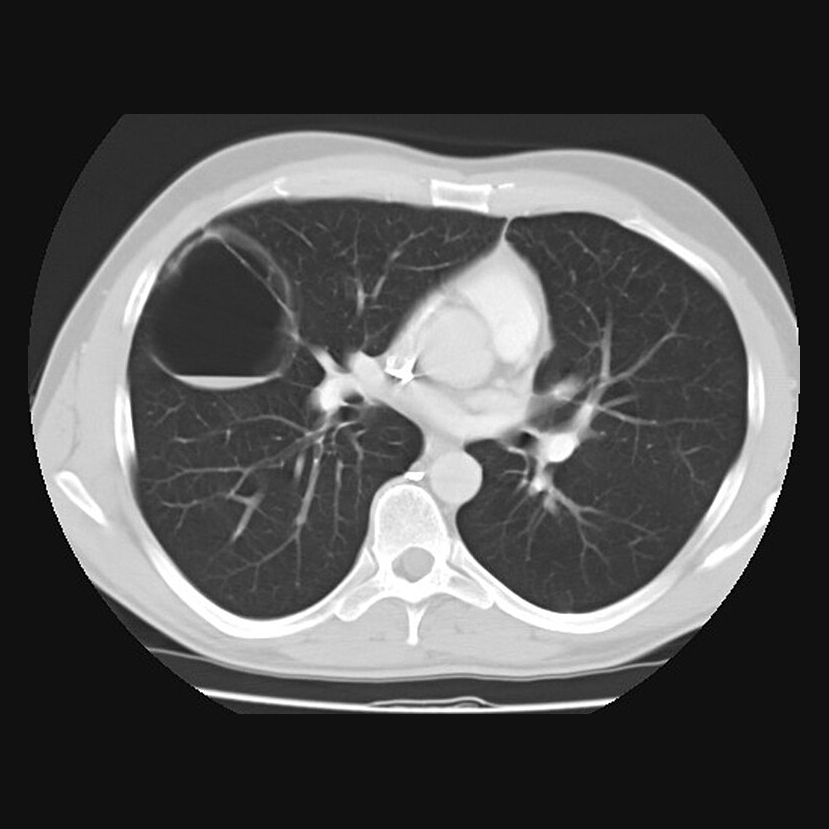
- High-resolution CT scan of the chest – to look for bronchiectasis
- Sputum cultures – to identify any bacteria in the lungs
- Sweat chloride test and/or genetic testing – to rule out Cystic Fibrosis
- Nasal nitric oxide testing, high-speed video microscopy – for Primary Ciliary Dyskinesia
- Blood tests – to check for immune system deficiencies
- Lung function testing – to assess how well the lungs are working, often done repeatedly over time
Treatment of Chronic Suppurative Lung Disease
While CSLD cannot always be cured, it can usually be effectively managed to improve quality of life, prevent flare-ups, and protect lung function. Management focuses on airway clearance, infection control, and treating the underlying cause.
Core components of treatment include:
- Chest physiotherapy and airway clearance
Daily physiotherapy is essential to help clear mucus from the lungs. Techniques may include percussion, breathing exercises, and devices like oscillating PEP. - Inhaled therapies
These may include bronchodilators to open the airways or nebulised saline to help loosen mucus. - Antibiotics
Oral or intravenous antibiotics are used to treat infective flare-ups. Long-term or inhaled antibiotics may be considered in some children with frequent exacerbations or chronic bacterial infection (e.g. Pseudomonas aeruginosa). - Treatment of underlying conditions
- Cystic fibrosis: specialist CF care
- PCD: coordinated respiratory and ENT management
- Immune deficiencies: replacement therapy or immune support
- Aspiration: dietary modifications or speech & language therapy input
- Vaccinations
Ensuring your child is up to date with routine and recommended vaccines (e.g. influenza, pneumococcal) helps prevent further infections.
Outlook and Follow-Up
Children with CSLD need regular follow-up with a paediatric respiratory team. With early diagnosis, tailored treatment, and good adherence to physiotherapy, many children experience:
- Fewer chest infections
- Improved energy levels
- Better school attendance and growth
- Slowed or even halted progression of bronchiectasis
Some children may show reversible changes, especially if treatment starts early.
When to Seek Medical Help
Contact your child’s medical team if you notice:
- Increased cough or change in colour/amount of sputum
- Fever or signs of infection
- Reduced exercise tolerance
- Weight loss or poor appetite
Prompt treatment of infections helps prevent further lung damage.
We offer expert evaluation and ongoing care for children with chronic cough, recurrent chest infections, and suspected CSLD or bronchiectasis
Located in London | Infants to young adults seen
Request a referral or book an appointment with Professor Gupta today.
